Augmented reality-assisted systematic mapping of anterolateral thigh perforators | BMC Musculoskeletal Disorders | Full Text
The GE medical systems revolution CT (GE Healthcare, Waukesha, WI, USA) was utilized in our study (Fig. 1A), and the parameters are as follows (Fig. 1B): 70 kVp, 500 mA, gantry rotation time of 1.0 s, and matrix 512 × 512. The patients were given 0.5 mg of sublingual nitroglycerin (Xinyi Corporation, Shandong, China) before the CT scan to appropriately dilate the perforators. During the examination, the patients were placed in the supine position, while iodinated contrast medium (100–120 ml) was injected at a rate of 5.0 ml/s into the antecubital vein (Fig. 1C). A region of interest ranging from the ASIS to the patella was selected to reveal the whole view of the ALTP, and the slice width was set as 0.625 mm to obtain the acquired volumetric data. Then, the images were transferred to a Philips Intelli Space Portal (Philips, N.V. Netherlands) automatically, and various required three-dimensional (3-D) images were generated to display the descending branch and its perforators (Fig. 2A, B). Moreover, different Hounsfield unit (HU) values of various tissues and calibres of vessels were detected (Fig. 2C, D). Principally based on the transverse images, the emergence points of the perforators from the muscle or intermuscular septum were marked and could be synchronously displayed in the coronal, sagittal and 3-D CTA images. Moreover, to reveal the emergence point of the ALTP more directly, image processing was performed to preserve the quadriceps femoris, and the subcutaneous fat tissue was removed (Fig. 3). Finally, these marked images were imported to the portable projector for the preoperative depiction of the ALTPs.
The prepared CTA images (Fig. 4A, B) were imported into the portable projector (XE11F, XGIMI Co., Chengdu, China), and the bony markers (the outline of ASIS and patella) in the images were projected coincident with the premarked bone contours (Fig. 4C). During this process, the position of the projector could be adjusted manually to align the ASIS and patella in the virtual map with the markers in the real surgical field. The projector could automatically adjust the focal length. At this time, the course of the LCFA and its descending branches was depicted on the skin surface, while the emergence points indicating the origin of the perforators from the deep fascia were also marked on the anterolateral thigh. Thus, the intraoperative ALTP flap area was designed to ensure sufficient blood supply (Fig. 4D).
Before the operation, the descending branch of the LCFA and its perforators, as well as the emergence points, were marked and depicted on the lateral thigh. Following disinfection and draping, the soft tissue defect was first measured. Then, the potentially contaminated area of each recipient was immediately wrapped with a sterile cloth to avoid cross-infection. The flap was designed with the consideration of the localized emergence points of the perforators to guarantee sufficient blood supply to the ALTP flap. Afterwards, the skin and subcutaneous tissue were incised along the internal or lateral edge of the predesigned flap until reaching the deep fascia. Then, the subcutaneous tissue was carefully separated under a microscope, identifying the perforators based on the premarked emergence points and preserving the soft tissue sleeve of all perforators (Fig. 5). Moreover, every distance between the premarked points and intraoperative findings was measured. Briefly, at the point where the perforators arising from the deep fascia were discovered during the operation, a vascular clamp was used to make a small protrusion on the skin surface. Hence, the distance between the protrusion point and the pre-marked point (whether by the Doppler or CTA&AR method) was measured to determine the accuracy of the preoperative localization. After all the perforators were separated, the descending branch of the LCFA was revealed along with the intermuscular space between the rectus femoris and lateralis muscle. The perforators of the descending branch, including the musculocutaneous and septocutaneous perforators, were separated posteriorly, while the redundant perforators were ligated to harvest the ALTP flap.
As shown in Table 1, of the 14 patients, 13 (92.9%) were male, and 1 (7.1%) was female, with a mean age of 50.8 years. Among them, 13 patients had severe open injuries of the lower extremities (Gustilo IIIB, IIIC), and only 1 had scarring of the hand. Half of them had a Mangled Extremity Severity Score (MESS) less than 7, and the other half of the patients had scores greater than 7, meeting the criteria for amputation. However, the patients opted for an ALTP flap to repair the large soft tissue defect to preserve the damaged limb. Postoperatively, patient 12 had a mixed infection, in which the causative bacteria were Enterobacter cloacae and Proteus vulgaris, because of the heavily contaminated wounds. Fortunately, the wound was largely healed after dressing changes were performed for approximately 1 month.
Number of emergence points acquired from imaging techniques and intraoperative findings
After the CTA examination and volume rendering, possible perforators emanating from the descending branch of the LCFA were meticulously identified on every transverse section, and then the emergence points were marked. A total of 55 and 38 emerging points were identified by CTA and Doppler ultrasound in 14 patients, respectively. Among them, CTA and ultrasound found 41 and 34 emergence points in the predesigned flap area, respectively, while 38 emergence points were found intraoperatively (Table 2). In the 14 patients, most of them had 2 (N = 6) or 3 (N = 7) ultrasound-located points, while the number of CTA-detected points was predominantly 3 (N = 5) and 4 (N = 5). The differences between the intraoperative findings, and ultrasound findings were greater but not statistically significant (P = 0.22), and the difference between the CTA and intraoperative findings were also not statistically significant (P = 0.852) (Table 3).
ALTP emergence points information
Verified by intraoperative findings, the emergence points depicted by handheld Doppler ultrasound and CTA were estimated by statistical methods (Table 4). In brief, although a total of 38, 55 emergence points were explored by ultrasound and CTA, some emergence points were not explored intraoperatively because they were beyond the predesigned flap area. Respectively, Doppler ultrasound and CTA found 34 and 41 emergence points that could be intraoperatively identified. Of the 34 points localized by ultrasound, 6 were not included because they were too far away from the intraoperative findings (> 3 cm), whereas the other 28 points were identified as valid emergence points of the perforators. Ten of the 38 emerging points found intraoperatively were not detected by Doppler ultrasound. Thus, the accuracy of handheld ultrasound was 82.4% (28/34), and the sensitivity was 73.7% (28/38). In contrast, 4 of the 41 points localized by CTA were not confirmed intraoperatively, while the other 37 points were identified as valid emergence points of the perforators. Moreover, among the 38 points that were found intraoperatively, only one point was not found preoperatively by CTA. Therefore, the accuracy of the CTA & AR projection method was 90.2% (37/41), and the sensitivity reached 97.4% (37/38).
The distances between the preoperatively marked points and actual emergence points found intraoperatively were considered another important indicator for the accuracy assessment, and these data are listed in Table 5. The 28 points marked by handheld ultrasound were 1.97 ± 0.50 cm from the intraoperatively detected points, while the locations marked by CTA were much more accurate (P < 0.001), with a difference in distance of 0.53 ± 0.27 cm. Moreover, the distance variances were significantly smaller in the CTA group than in the ultrasound group; an F test to compare variances revealed a value of 3.359 (P = 0.0372). Thus, the emergence points obtained by the CTA & AR projection technique were more accurate than those obtained by Doppler ultrasound.
Flap survival and follow-up
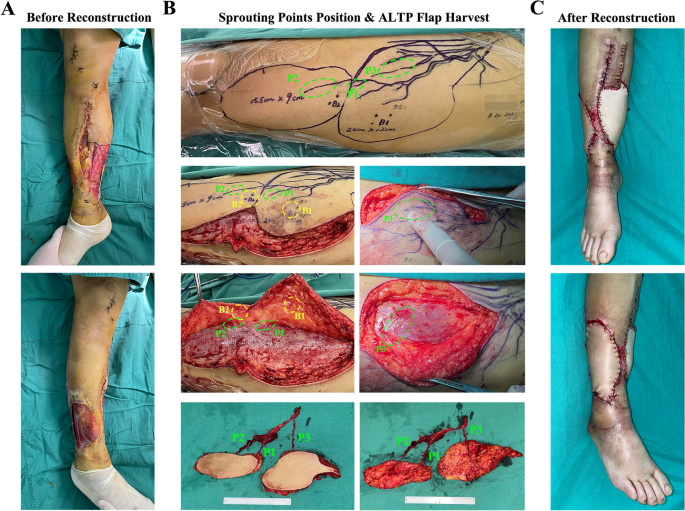
In the 14 patients, all ALTP flaps were successfully used to reconstruct soft tissue defects in the damaged limbs, with two patients suffering from complications, including partial flap necrosis and mixed infections (Table 1). In Figs. 6 and 7, two typical cases are displayed to illustrate the specific procedure and results of the CTA & AR projection technique applied in the clinic. Briefly, Fig. 6 shows the treatment procedure of patient 9. After thorough debridement, there were large soft tissue defects on both the medial and lateral sides of the right calf, with tendon and bone exposure. Moreover, the medial and lateral wounds were connected by a posterior subcutaneous tunnel. The wound was defined as Gustilo IIIB with a MESS of 6 points. After the preoperative CTA examination, a total of 3 emergence points of the ALTPs were marked, while 2 points were localized by Doppler ultrasound. Then, the flap was designed according to the preoperatively localized points, and the accuracy of these points was evaluated by intraoperative flap harvest. During the operation, a 15.5*9.0 cm and 22.0*12.0 cm double-leaf ALTP flap was obtained to repair the soft tissue defect in the right calf. Ultimately, the ALTP flap survived, and no related complications occurred. In another case, Fig. 7 shows the treatment procedure for patient 12. The right dorsal foot of this patient was unfortunately strangulated by a machine for chicken farming and was mixed with numerous chicken droppings, grains, and dirt. No improvements occurred after several debridements, and a soft tissue defect of approximately 18*5.5 cm was present on the dorsum of the right foot, with a dorsalis pedis artery defect and metatarsal exposure. Overall, the wound was defined as Gustilo IIIC with a MESS of 10 points. The bacterial culture showed a multidrug resistant mixed bacterial infection (Enterobacter cloacae & Proteus vulgaris). After thorough debridement, CTA was performed, and 4 emergence points (points A-D) of the ALTPs were marked, of which the thickest perforator was point A. Accordingly, the ALTP flap was designed and depicted on the skin surface, encompassing 3 ultrasound-located points. During the operation, a thick perforator emerging from the deep fascia under CTA-marked point A (indicated by the forceps) was seen to converge into the descending branch of the LCFA, whereas the ultrasound-marked perforators mostly continued into the transverse branch or traffic branches emanating from the deep femoral artery. Simultaneously, a portion of the rectus femoris and its corresponding musculocutaneous artery was obtained along with the flap to fill the foot defect, with the aim of controlling the severe infection. The flap eventually survived, but the wound continued to exude yellowish fluid after the operation, probably due to the bacterial infection. After being treated with anti-infection drugs and daily dressing changes, the wound healed completely after one month.
A typical case of a 52-year male. A After debridement, large soft tissue defects on the medial and lateral sides of the right calf existed, accompanied by tendon and bone exposure. B The location of the emerging point (P1-P3) came out from the deep fascia and the real-time perforators mapping were depicted on the anterolateral skin of the left thigh according to the prepared CTA images. Meantime, the pulse point of perforators (B1-B2) was also marked on the skin surface using handheld Doppler ultrasound. During operation, the lateral edge of the flap was cut up, and the cutaneous branches around the emerging points were carefully separated. It should be noticed that the emerging points of the perforators were in accordance with the preoperative marked locations determined by AR, while the points located by ultrasound were far away from the perforators. Finally, a double-foliate ALTP flap containing three perforators was obtained. C The damaged calf was reconstructed by the ALTP flap
A typical case of a 52-year male. A After debridement, large soft tissue defects on the medial and lateral sides of the right calf existed, accompanied by tendon and bone exposure. B The location of the emerging point (P1-P3) came out from the deep fascia and the real-time perforators mapping were depicted on the anterolateral skin of the left thigh according to the prepared CTA images. Meantime, the pulse point of perforators (B1-B2) was also marked on the skin surface using handheld Doppler ultrasound. During operation, the lateral edge of the flap was cut up, and the cutaneous branches around the emerging points were carefully separated. It should be noticed that the emerging points of the perforators were in accordance with the preoperative marked locations determined by AR, while the points located by ultrasound were far away from the perforators. Finally, a double-foliate ALTP flap containing three perforators was obtained. C The damaged calf was reconstructed by the ALTP flap
A typical case of a 56-year female. A Four marked emerging points A-D were showed in CTA images, but only one point was in the designed ALTP flap area. B During operation, the preoperatively marked point A was just above the emerging point of the perforator (green arrow). C The harvest ALTP flap and vascular pedicle. D After debridement, the damaged foot with 18.0 cm * 5.5 cm soft tissue defect was reconstructed by the ALTP flap
This content was originally published here.